Frontotemporal dementia, or FTD, is a neurodegenerative condition that mainly affects how people speak, behave, and move. Unlike other types of dementia, it usually shows up earlier in life; most often between the ages of 45 and 65.
Because it starts earlier and impacts important abilities of an individual, having a clear understanding of the 7 stages of frontotemporal dementia (FTD) can be especially helpful. This knowledge will support both the individuals living with the condition and their caregivers. It makes it easier for them to prepare for what’s ahead and provide the best care possible.
Let’s discuss the 7 stages of FTD and explore what you can expect at each stage, both as an individual and as their caregiver.
What is Frontotemporal Dementia?
FTD is a consequence of abnormal protein deposition in the frontal and temporal lobes of the brain. These regions define languages and behavioral expressions, which is why most patients suffering from FTD typically exhibit symptoms of speech and personality. The cause of FTD cannot be determined; however, it is familial. Studies show that out of 42 people with FTD, 19 people (about 45%) had at least one family member who also had an FTD-related condition. This means almost half of the cases were family-related. You should search for memory care facilities near me to provide the specialized support needed for individuals facing these challenges.
Check out the link to learn more about memory care services, their costs, benefits, and services.
Brain Impact
- Frontal Lobe: Governs behavior and personality.
- Temporal Lobe: Controls language and memory.
- Protein deposits damage these areas, causing FTD symptoms.
If someone in your family is showing early signs, learning about the 7 stages of frontotemporal dementia can help you catch it early and plan ahead.
Symptoms of Frontotemporal Dementia
FTD is characterized by a range of progressive symptoms, including:
|
Symptom Type |
Common Examples |
|
Personality & Behavior |
Apathy, impulsivity, emotional lability |
|
Language |
Word-finding difficulty, slow or unclear speech |
|
Cognitive |
Distractibility, difficulty with daily tasks |
|
Motor |
Weakness, swallowing difficulties, and coordination loss |
How is a brain with FTD different from a Normal Brain?
Each part of the brain has its own job to do, like controlling how we talk, behave, move, and remember things.
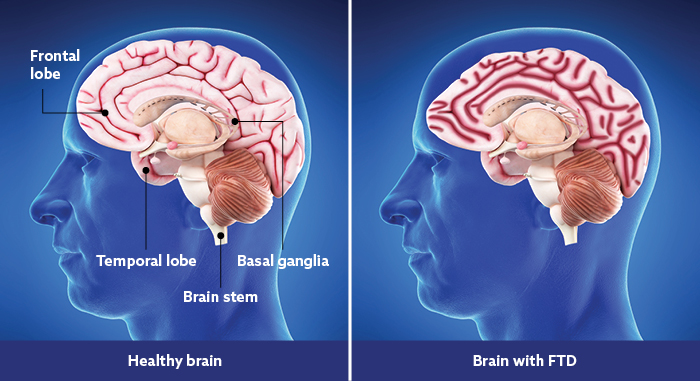
In FTD, some of these important parts get smaller and damaged, which leads to the symptoms people notice.
Let’s take a look at what’s different.
|
Brain Part |
Healthy Brain |
Brain with FTD |
| Frontal lobe | Helps with personality, making decisions, and how we behave. | Gets smaller, which causes changes in behavior and personality. |
| Temporal lobe | Helps with language, memory, and hearing. | Shrinks, leading to trouble with talking and remembering. |
| Basal ganglia | Controls movement and coordination. | Mostly stays okay, so some movement control is still good. |
| Brain stem | Connects the brain to the spinal cord and handles basic body functions like breathing and heartbeat. | Usually stays healthy, so basic body functions keep working well. |
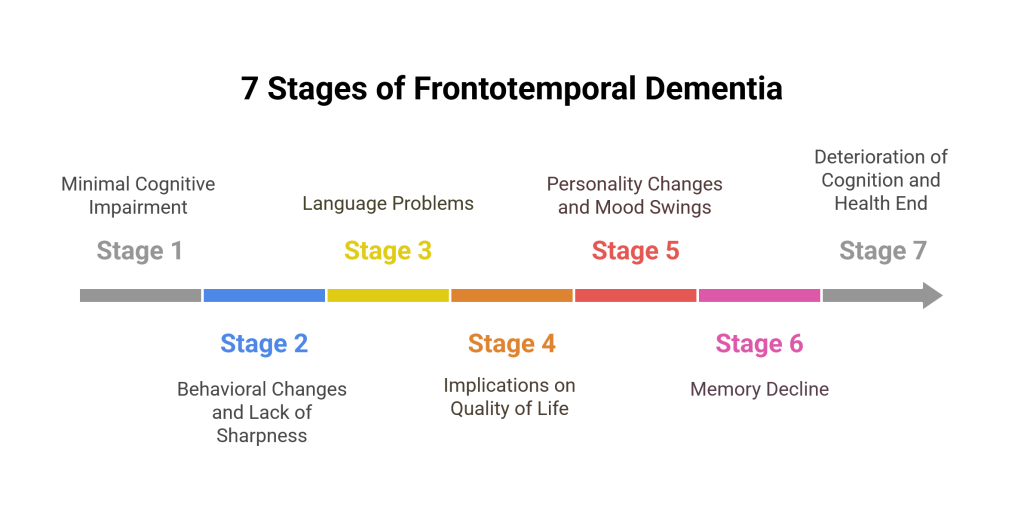
7 Stages of Frontotemporal Dementia
FTD progresses gradually through seven consecutive stages. Some people will not develop into stage seven, and the pace of advancement varies with different people.
Stage 1: Minimal Cognitive Impairment
At this stage, FTD is very covert. Patients may only realize them once the effects have already become significant. Most patients may experience unusual behaviors, trouble with speaking, or acting a bit withdrawn. At this stage, their memories are not that affected. It does not grossly affect their quality of life, so people may not associate those behaviors with a neurological disease.
Stage 2: Behavioral changes and Lack of Sharpness
During this period, slight behavioral changes and acuteness of the mind are visible. An individual struggles to find the right words and performs odd or antisocial behavior. From these subtle changes, people may get an initial indication to detect FTD and how it gradually affects social or professional life.
Stage 3: Language Problems
The symptoms are steady and progressive in the middle-stage FTD. The person starts facing language problems that affect his work and personal relationships. The person may need to be made aware of this change, but outsiders typically notice these changes. There is a decline in home and work life.
Stage 4: Implications on Quality of Life
At this stage, symptoms are very oppressive to the quality of life. Speech deteriorates, and people cannot remember to use simple sentences in memory. More classic symptoms of dementia, such as forgetfulness and limitations in carrying out daily activities, often appear at this level. Driving and staying in places with which they are unfamiliar becomes burdensome.
Stage 5: Personality Changes and Mood Swings
The mid to late stages of frontotemporal dementia (FTD) affect daily living a lot. People may face big mood swings and personality changes. Their language, memory, and problem-solving weaken. Movements get stiff, making limb use harder. Caregivers play an important role at this stage among the 7 stages of frontotemporal dementia. They assist daily and ensure safety and support.
Stage 6: Memory Decline
Late-stage FTD is very similar to Alzheimer’s dementia. Language and behavior are radically impaired, and the loss of memory results in extreme mental deterioration. The patient may be isolated inside himself, with little emotional, bodily, or verbal expression. Motor disturbances, including balance and reflex, make falls and accidents common. You can address the emotional toll of Dementia care by opting for a few strategies.
Stage 7: Deterioration of Cognition and Health End
At the final stage of FTD, thinking and memory issues get very serious. The general health of the individual also suffers, and thus, the individual needs lots of attention and assistance. Respiratory illnesses, pneumonia, and other severe illnesses are common. Additionally, because the patients are likely to fall or be injured, it becomes hard for them to recover and stay healthy.
Stage Highlights
- Early Stages (1-2): Subtle symptoms often overlooked.
- Mid Stages (3-5): Daily life and independence are heavily impacted.
- Late Stages (6-7): Complete dependence and medical support are essential.
Family & Caregiver Impact During the 7 Stages of Frontotemporal Dementia
FTD can be tough on families. A study of 102 caregivers of people with frontotemporal degeneration found that apathy in patients caused more stress for caregivers. The main reason is the stronger behavioral symptoms and trouble speaking, which makes it hard to care for and connect with loved ones.
- Big behavior changes: FTD can cause someone to act in ways that seem strange or even scary, which can really shake loved ones.
- Trouble communicating: As speech becomes harder, everyone struggles with the loss of normal talking.
- Emotional strain: Seeing a loved one change so much can feel like a slow goodbye.
- Isolation: Caregivers can feel left behind, especially if no one knows what they’re really facing.
- Burnout risk: Stress, tasks, and strong emotions can drain anyone, even the most patient.
- High caregiver burnout: More burnout in FTD caregiving shows why breaks and emotional support are vital now.
Higher burnout rates in FTD caregivers underscore the need for emotional support and respite care.
Treatment Options Across the 7 Stages of Frontotemporal Dementia
Frontotemporal dementia is a progressive disease that has no cure. Nevertheless, there are a few interventions that may be used to relieve symptoms and enhance the quality of life of patients and caregivers. Some of these common methods are listed below and they include medications, therapies, and support options.
Medications
- Antidepressants: These are often prescribed to help with behavioral symptoms such as depression, anxiety, and irritability. Common examples include fluoxetine (Prozac), sertraline (Zoloft), and citalopram (Celexa).
- Antipsychotics: In more severe cases, antipsychotic drugs may be used to control agitation, aggression, or psychosis. These medications should be used carefully, as they can have serious side effects, especially in older patients. Risperidone (Risperdal) and olanzapine (Zyprexa) are among the commonly prescribed options.
- Cholinesterase Inhibitors and NMDA Receptor Antagonists: These medications are typically prescribed to treat Alzheimer’s disease, but in some cases, they may be prescribed to treat cognitive symptoms in patients with FTD. Examples are donepezil (Aricept) and memantine (Namenda).
Therapies
- Speech Therapy: Speech therapists work with people with FTD to improve their ability to communicate. This may involve using gestures, communication devices, or other methods to make speaking clearer.
- Occupational Therapy: Occupational therapists support people in doing everyday tasks. If someone has trouble thinking or moving, they offer ideas, tools, or home fixes to make life easier and safer.
- Physiotherapy: Physical therapy addresses motor symptoms and provides mobility. Physicians prescribe activities that address the patient’s mobility problem. Exercises like these are designed to enhance your strength and balance, so that you are less prone to falling or injuring yourself as you continue with your day.
A combination of drugs and treatment can make symptoms manageable, and, unfortunately, they do not prevent the development of the disease.
Caregiving Strategies for Managing FTD
Caregiving to a person with FTD is a demanding task, and these few tips may make it easier. Safe homes and clear routines make days less stressful.
Establish Consistent Routines To Minimize Confusion
Having a routine helps the person feel safe and reduces confusion. Keep activities and meals steady.
Use Clear, Simple Language With Patience
Use short and clear words. Speak slowly and give time to respond. Patience helps with talking.
Modify The Home For Safety
Make changes like grab bars and clearing clutter to keep things safe and avoid falls.
Promote Appropriate Physical Exercise
Light exercises like walking should be advised so that they are active and in a better mood.
Connect with Caregiver Support Groups to Reduce Isolation
Support groups let you connect with others and share your experiences.
Get Support Through All 7 Stages of Frontotemporal Dementia!
Understanding the seven stages of FTD can help predict problems ahead of time and provide the needed support for FTD patients. Generally, there is no cure for this disease; however, early diagnosis and intervention can control and possibly manage the symptoms of the disease, from the establishment of a life entirely of hopelessness.
Sierra Oaks provides advanced care and choices for treating patients, providing assistance, and the best available care and support. Search for memory care facilities near me, and let Sierra Oaks guide you with the best care options.